Share Article
As of January 1, 2025, the Centers for Medicare & Medicaid Services is rolling out an exciting new opportunity for primary care providers through Advanced Primary Care Management (APCM) services. With three new HCPCS codes, providers can now streamline billing and get rewarded for delivering comprehensive, high-quality care—not just time spent with patients. These codes bundle key services like Chronic Care Management (CCM), Principal Care Management (PCM), Transitional Care Management (TCM), and Communications Technology-Based Services (CTBS) into one simplified monthly payment based on the complexity of a patient’s condition.
In this blog, we’ll take a closer look at APCM: what the codes are, what is required from APCM, what the benefits are, and how you can support your APCM needs.
A strong foundational primary care system is fundamental to improving health outcomes, lowering mortality, and reducing health disparities, which is why the Department of Health and Human Services has been taking action to strengthen primary care, starting with payment for advanced primary care management services.
Centers for Medicare and Medicaid Services
What are the APCM Service codes?
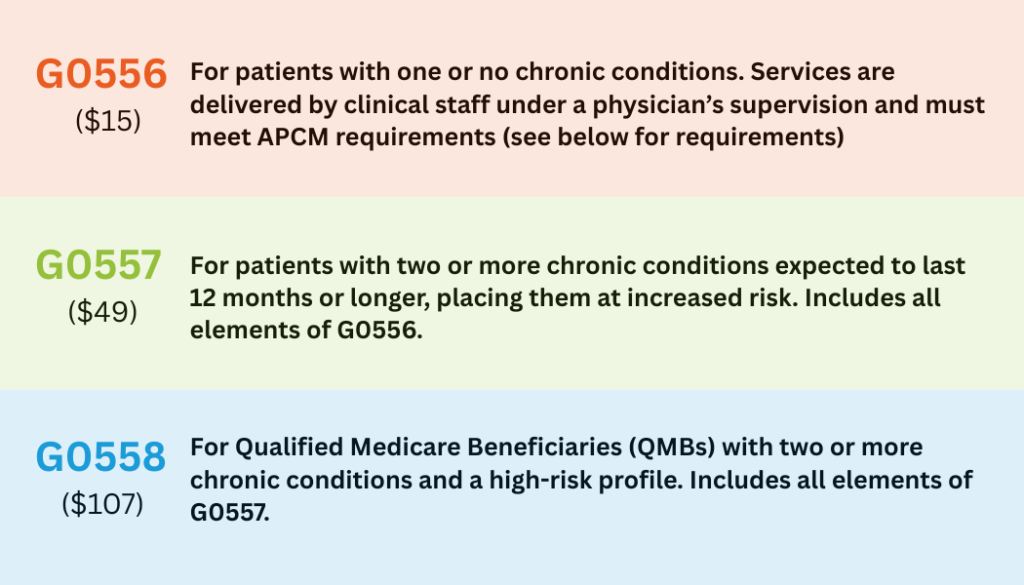
These services are billed per patient per month using these three HCPCS codes (national average reimbursement shown; may vary by region):
What’s Required to Bill for Advanced Primary Care Management?
To bill under any APCM code, providers must make 10 core service elements available to patients. The good news: providers are not required to deliver all 10 every month—services can be tailored based on patient needs.
Here’s what must be available:
- Consent: Explain the service, get patient agreement, and record it in their chart.
- Initiating Visit: Needed for new patients or if not seen in 3+ years (AWV may count).
- 24/7 Access: Round-the-clock contact with care team, real-time records, and same-team follow-ups.
- Care Management: Assess needs, provide preventive care, manage meds, oversee treatment.
- Care Plan: Keep a shared, up-to-date plan accessible to the care team and patient.
- Care Transitions: Arrange referrals, follow up after ER/hospital/SNF discharge.
- Home & Community Coordination: Work with outside providers and services to meet patient goals.
- Enhanced Communication: Use secure messaging, portals, and digital tools for remote care.
- Population Management: Use data to find care gaps and target high-risk patients.
- Performance Reporting: Track quality, costs, and participate in CMS value-based programs.
What is a Qualified Medicare Beneficiary?
A Qualified Medicare Beneficiary is a Medicare enrollee who qualifies for financial assistance to help cover Medicare costs due to having a low income or limited resources. A patient who identifies as a QMB and has two or more chronic conditions qualifies for reimbursement Code G0558. To find out if a patient is in the QMB program, either use the HIPPAA Eligibility Transaction System or contact your Medicare Administrative Contractor’s Online Provider Portal.
Who Can Bill for Advanced Primary Care Management Services?
APCM services should be provided by the primary care provider or the first point of contact for the patient’s general health needs. APCM services can be provided by: physicians, nurse practitioners, physician assistants, and clinical nurse specialists. Federally Qualified Health Centers and Rural Health Clinics are also eligible to participate under the guidelines.
What Are the Benefits of Advanced Primary Care Management for Providers and Patients?
How Does this Initiative Support Value-Based Care?
APCM is more than just a billing model—it represents a meaningful shift toward value-based care. Unlike CCM and PCM, APCM codes are not time-based, allowing practices to bill for care management activities that may not meet the 20- or 30-minute thresholds required by other programs.
Advanced Primary Care Management codes are also stratified into three levels, based on the number of chronic conditions a patient has and whether the patient is a Qualified Medicare Beneficiary. This model helps reflect patient support for those affected by various social determinants of health.
By promoting continuous, comprehensive, and patient-centered care, Advanced Primary Care Management aligns financial incentives with better health outcomes, improved population health, and a reduction in avoidable healthcare utilization.
APCM stands apart from other care management services as it must be driven by the patient’s primary provider, categorizes patients by need level, and uses quality measures to assess program effectiveness.
National Association of Community Health Centers
How does APCM integrate with RPM?
Advanced Primary Care Management supports ongoing care, designed to help patients live longer, healthier lives. Remote Patient Monitoring uses medical devices, like blood pressure machines, to track patients’ vital signs remotely, giving providers a clear, real-time picture of their health.
Imagine a patient enrolled in APCM for diabetes and hypertension. With an RPM program in place, their blood pressure is monitored daily and remotely. If a spike is detected, a care management team can quickly intervene, providing support and instruction to mitigate the risk. Because RPM services like ongoing monitoring, patient communication, and care plan management align with APCM service elements, integrating RPM into your APCM workflow not only enhances patient care—it also helps meet CMS requirements more efficiently.
How Netrin Can Support Your APCM Program
Navigating the requirements of APCM on your own can be complex – but you don’t have to do it alone. Value-based care partners like Netrin Health can deliver elevated support to make a successful APCM program. Under the supervision of a billing provider, our care team handles all the requirements of the APCM that might be time-consuming for your direct clinical staff.
Partnering with Netrin means more than just meeting the requirements. We go above and beyond to bring you comprehensive care management, data collection for population health assessments, an efficient RPM program, updating patient-centered plans, and ensuring 24/7 access to care for your patients. Our experienced team—including nurses, care managers, social workers, and more—is ready to help your practice streamline workflows, improve patient outcomes, and maximize APCM reimbursement.
