Share Article
Have you ever had to make difficult medical decisions for yourself or someone else?
During a medical emergency or at the end of life, you may face questions about the medical treatment for your loved ones. In fact, studies show that up to 75% of people will need someone to help make medical decisions at some point in their life. Another study shows that people guessed nearly one out of three end-of-life decisions for their loved one incorrectly.
Being asked to guess your loved one’s end-of-life wishes after they become incapacitated is challenging. Yet preparing ahead of time can decrease the stress, burden, and disagreement experienced by those who need to make medical decisions for you, while ensuring that health care treatment you may receive is consistent with your wishes and preferences.
What is Advance Care Planning?
Advance Care Planning (ACP) is the preparation for communication and medical decision-making. The process supports adults at any age and at any stage of health in understanding and sharing their life goals, values and preferences regarding their current and future medical care.
Patients are more likely to get the care they want if they have conversations about future medical treatments and put a plan in place. That’s why patients, caregivers, and medical providers should talk about Advance Care Planning before a medical crisis occurs.
Who Needs an Advance Care Plan?
Advance care planning is not just for people who are very old or ill. At any age, a medical crisis could leave you unable to communicate your own health care decisions. Planning now for your future health care can help ensure you get the medical care you want and that someone you trust will be there to make decisions for you.
What are Advance Care Directives?
While advance care planning is the process of planning for future care, an advance care directive is the record of that process. Advance care directives are legal documents that provide instructions for medical care and only go into effect if you cannot communicate your own wishes.
The living will and the durable power of attorney for health care (DPAHC) are the two most important components of advance care directives.
Living Will vs Durable Power of Attorney for Health Care (DPAHC)
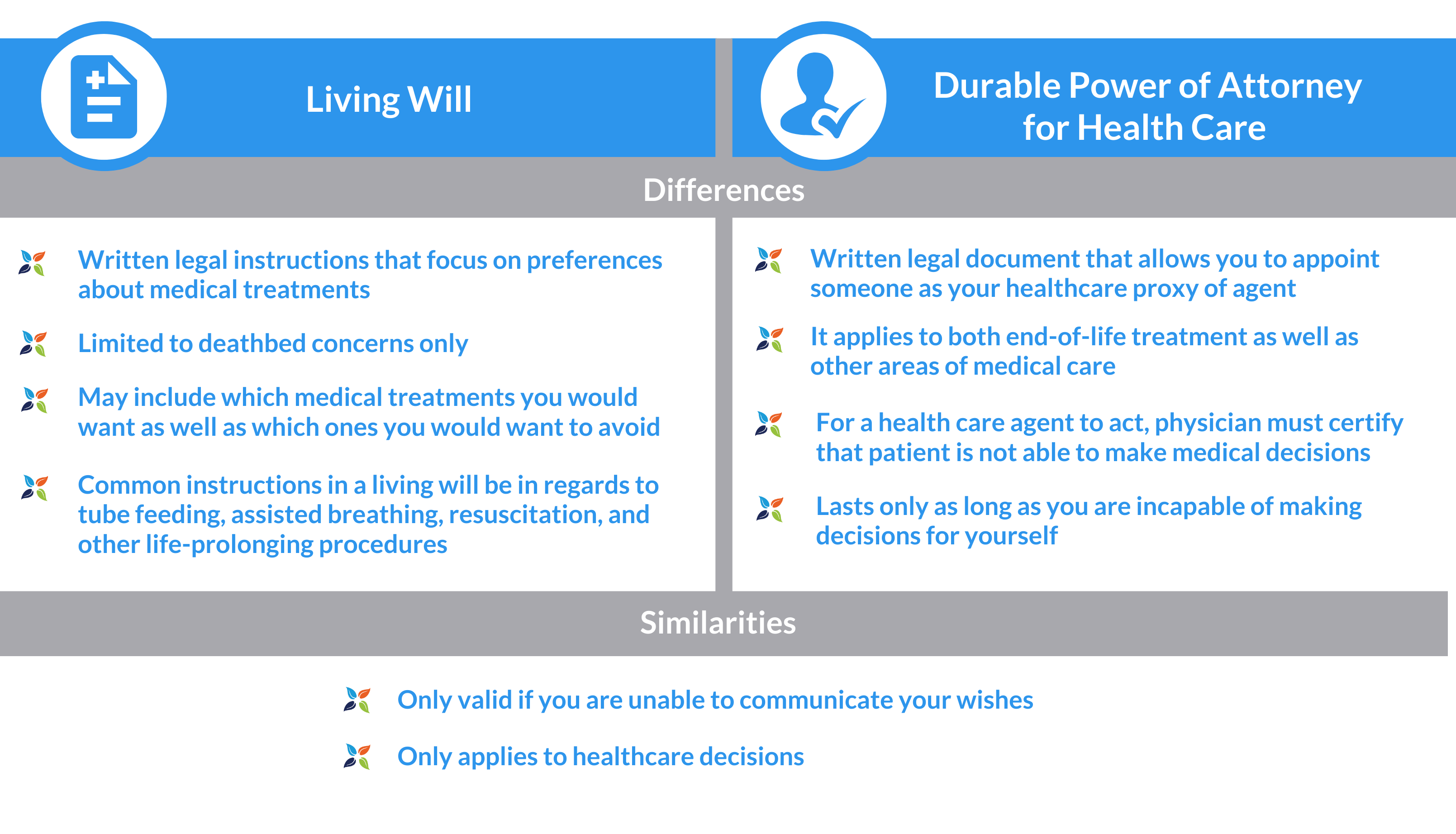
You can choose a durable power of attorney for healthcare in addition to, or instead of a living will. If you decide to have both, a durable power of attorney and a living will, it is called combined advance directives for health care. It’s often recommended that your plan is as comprehensive as possible, therefore having both as part of your advanced care planning.
Living Will: What End-of-Life Issues Does it Cover?
As part of a patient’s advance care directives, a living will tells your healthcare providers the medical treatments you may or may not want, if you’re permanently unconscious or at the end of a terminal illness. It may include how long you want your life prolonged as well as your religious preferences.
Living wills specifically express your preferences for medical treatments, and may include the following.
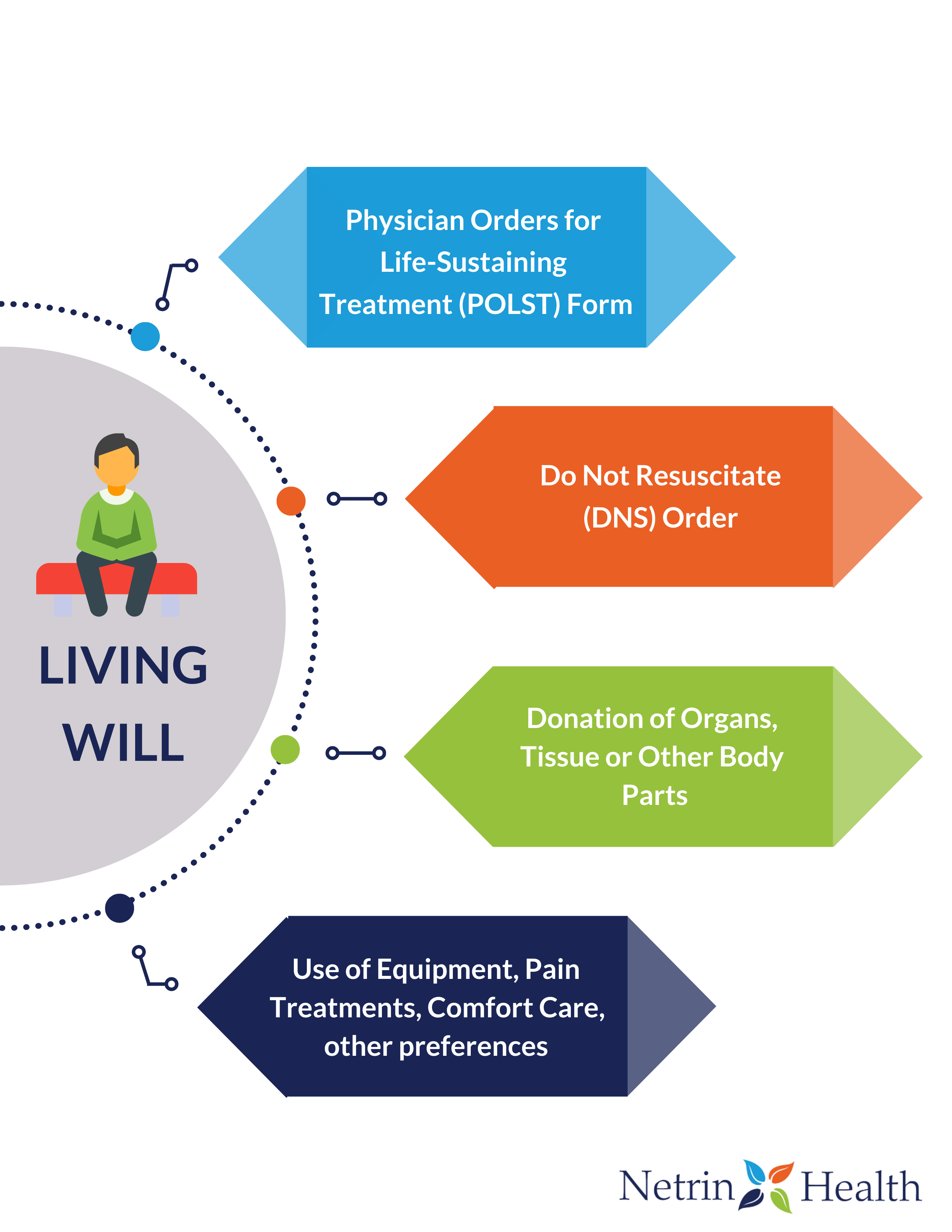
- Physician Orders for Life-Sustaining Treatment (POLST)
POLST is part of advance care planning intended for people who are seriously ill or who have advanced frailty. A POLST Form complements the advance care directive — it does not replace it. It consists of medical orders that tell emergency health care professionals what to do during a medical crisis where the patient cannot speak for him or herself.
Orders on a POLST form include:
- Whether you want cardiopulmonary resuscitation (CPR) attempted
- Whether you want to go to the hospital or stay where you are
- Whether you want to receive care in an intensive care unit and be on a breathing machine, if needed
- Do Not Resuscitate (DNS) Order
A Do-Not-Resuscitate (DNR) order instructs the medical staff not to enact life-saving measures such as cardiopulmonary resuscitation (CPR) or an automated external defibrillator. It is specific about CPR in case the patient’s breathing stops or if the patient’s heart stops beating. It does not have instructions for other treatments, such as pain medicine, other medicines, or nutrition.
- Other End-Of-Life Decisions
Advance care directives can also include other decisions about end-of-life care, including;
- Whether you want the use of equipment such as dialysis machines (kidney machines) or ventilators (breathing machines) to help keep you alive
- Whether you want treatment for pain, nausea, or other symptoms, even if you can’t make other decisions (this may be called comfort care or palliative care)
- Whether you wish to donate organs, tissues, or other body parts
Advance Directives are State-Specific
Every state allows for certain types of advance care directives, so it’s important to check the state approved advance directive documents before completing advance directives. The laws in every state can vary – for instance, some states allow verbal advance directives while others do not.
Also if you spend most of your time in more than one state, be sure to speak to your health care provider and review each of the states’ laws.
Advance directives are living documents, and it’s recommended that you review them at least once each year, and update if a major life event occurs – such as retirement, moving out of state, or a significant change in your health.
Advanced Care Planning for Medicare Patients
The Centers for Medicare and Medicaid Services (CMS) allows Medicare to pay physicians and other qualified health care professionals for providing ACP consultation to beneficiaries.
This Medicare benefit helps to allow senior patients to have the opportunity to discuss their treatment preferences with a health care provider, regardless of their economic or personal resources. If you are discussing ACP with your doctor during your Annual Wellness Visit, you will not owe a copayment or deductible.
Everyone should consider advance care planning, regardless of their age or health. But it is particularly important if you:
- are 65 or older
- have a chronic illness
- have multiple diseases
- have an early cognitive impairment
- are approaching the end of your life
Start the Conversation Today
For the many older Americans living today with one or more chronic conditions, advance care planning is an important part of chronic disease self-management. But no matter what your current state of health, now is the time to prepare.
Advance care planning can be a gift you give yourself and your family. Planning ahead of time will relieve family members from wondering if they made the right choices on your behalf. To start the conversation about your own advanced care planning, schedule your Annual Wellness Visit and or talk to your doctor about advance care planning in your next appointment.
Silveira, M., Kim S., Langa K., Advance Directives and Outcomes of Surrogate Decision Making before Death. The New England Journal of Medicine.
Sudore R., Fried T., Redefining the “Planning” in Advance Care Planning: Preparing for End-of-Life Decision Making. NIH National Library of Medicine.
Sherry G., (March 14, 2020). 6 Characteristics to Look for When Choosing a Power of Attorney. Very Well Health.
