Share Article
Now is the time for every Medicare Shared Savings Program Accountable Care Organization (MSSP ACO) to get ready for the 2025 reporting deadline.
As part of the Quality Payment Program (QPP), MSSP ACOs will face new reporting obligations starting in 2025. Post the 2024 performance year, The Centers for Medicare and Medicaid Services (CMS) plans to transition entirely to digital quality measurement, requiring the reporting of eCQMs for all patients, payers, and health practices. The APM Performance Pathway (APP) is the fresh CMS reporting method for MIPS Alternative Payment Models (APMs) and ACOs, serving as a replacement for the CMS Web Interface.
Despite the expectation of a more streamlined reporting system, this shift poses challenges, particularly for ACOs that are not ready for the conclusion of the Web Interface era. In this article, we’ll talk about what these changes mean for ACOs, including the new APP quality measures and some practical strategies to help ACOs report successfully.
A Closer Look at the Current ACO Quality Reporting
ACOs traditionally reported 10 Quality measures using the CMS Web Interface. However, after the 2024 performance year, CMS will retire the Web Interface. ACOs will then need to report the 3 APP eCQMs/MIPS CQMs, which focus on diabetes, depression screening, and hypertension.
CMS has allowed a more extended transition period to provide ACOs with ample time to get ready for these modifications. ACOs can opt to continue reporting the 10 quality measures through the Web Interface until the end of performance year 2024. However, from 2025 onward, ACOs will be mandated to report all three eCQMs/MIPS CQMs.
What is The New APM Performance Pathway (APP)?
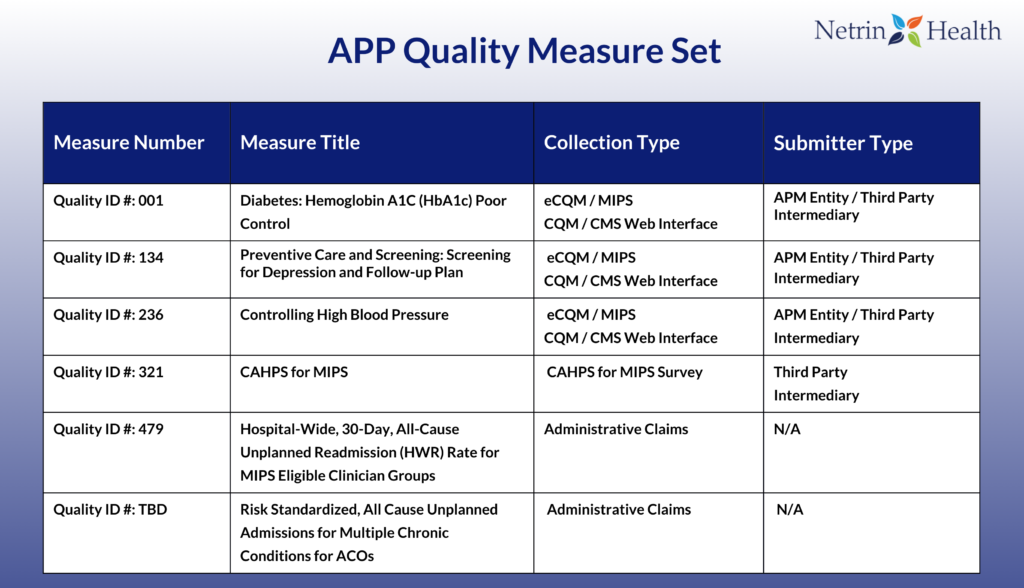
In the 2021 Final Rule for the Quality Payment Program (QPP), CMS introduced a new reporting process for MIPS Alternative Payment Models (APMs) and ACOs called the APM Performance Pathway (APP). The APP measure set will include the three self-reported Quality measures (eCQMs/MIPS CQMs), two measures calculated by CMS using administrative claims data and a patient experience measure.
The Quality measures included in the APP measure set focus on the management of chronic health conditions that have a high prevalence among Medicare beneficiaries and also the general population. CMS will require that the measures be reported for at least 70% of eligible patients regardless of payer type (both Medicare and non-Medicare patients) to assess the overall quality of care furnished by the ACO.
Description of the New Quality Measures
A description of each of the Clinical Quality Measures (CQMs) can be found below:
- Quality ID #1 (NQF 0059): Diabetes: Hemoglobin A1c (HbA1c) Poor Control (>9%)
This metric is documented for patients aged 18-75 with diabetes, focusing on those whose latest hemoglobin A1c level, assessed during the measurement period, exceeded 9.0%. Submission is required at least once per performance period. It is essential to recognize that this is an “inverse” measure, signifying that a lower calculated performance rate signifies superior clinical care or control. Opting for the “Performance Not Met” numerator option, which includes patients with an A1c level below 9%, results in a performance rate approaching 0% as the quality improves.
While CMS explicitly mentioned the two codes for RTM treatment management services, future inquiries could seek clarification on whether multiple practitioners can bill CPT codes 99457 and 99458 for the same patient within the same 30-day period.
- Quality ID #134 (NQF 0418): Preventive Care and Screening: Screening for Depression and Follow-Up Plan.
This metric involves reporting on individuals aged 12 and above who underwent depression screening either on the encounter date or within 14 days before the encounter, utilizing a suitable standardized tool. If the screening indicates a positive result, a follow-up plan must be documented on the eligible encounter date. Submission of this measure is required at least once within the measurement period.
- Quality ID #236 (NQF 0018): Controlling High Blood Pressure.
This metric is documented for patients aged 18 to 85 diagnosed with hypertension during the measurement period. It focuses on those whose most recent blood pressure was effectively controlled (< 140/90 mmHg) throughout the same period. Submission of this measure is required at least once per performance period for patients with hypertension who were seen during that period. It’s important to note that only blood pressure readings conducted by a clinician or a remote monitoring device are considered acceptable for complying with the numerator of this measure.
Reporting Methodology Changes for 2025
The New Measure Set
Although the new APP measure set is less extensive than the Web Interface measure set, there are notable differences in the quality reporting requirements. In the Web Interface, ACOs report quality measures for a subset of 248 Medicare patients per measure during the performance year. Conversely, with the APP measures, reporting is mandated for a minimum of 70% of all eligible patients, encompassing both Medicare and non-Medicare, throughout the performance year (January – December).
The New Quality Measure Benchmarks
Under the APP, ACOs’ quality performance scores will be computed using the same MIPS benchmarks applied to other non-ACO individual and group reporters. Each Quality measure is evaluated against its respective benchmark to determine the earned points. The benchmarks vary depending on the collection type under the APP, distinguishing between MIPS Clinical Quality Measures (MIPS CQMs) and Electronic Clinical Quality Measures (eCQMs). These benchmarks are set using historical data derived from actual performance data submitted to the QPP.
For measures meeting the data completeness and case minimum requirements, ACOs will receive a score ranging from 3 to 10 points. This determination is made by comparing measure performance to the established benchmarks, each expressed in deciles.
Navigating Data Aggregation
The revised APP reporting method mandates the aggregation of data from various sources before submission to CMS. This necessity arises from the considerably larger data sample required under this program. ACOs typically have data dispersed across various practices (Tax Identification Numbers or TINs), often involving multiple electronic health record (EHR) systems and billing platforms, adding complexity to the data collection process.
Choosing the Right Value-Based Care Partner
In anticipation of the removal of the CMS Web Interface, CMS is extending additional time for ACOs to set up systems and familiarize clinicians with upcoming quality reporting obligations.
Recognizing potential concerns about transitioning to a new measure set, adopting fresh reporting methods, and embracing all-payer reporting, we emphasize the importance of initiating preparations now and selecting a partner capable of providing strategies for a seamless transition.
Finding a value-based care partner with expertise in data aggregation and reporting is crucial for success. ACOs should start identifying a new data collection mechanism, adjusting operational workflows, and evaluating their performance on Quality measures. Fortunately, Netrin Health is prepared to facilitate this seamless transition and position ACOs for success in reporting.
If your organization is not fully prepared for this transition or requires assistance in navigating the intricacies of the new reporting requirements, Netrin Health is here to guide you along the way. Contact us today to schedule a consultation.
