Share Article
Hierarchical Condition Category (HCC) – a vital component of value-based care – plays a pivotal role in evaluating patients’ health conditions and projecting their future healthcare expenses. While the concept of HCC coding is not new, it’s getting renewed attention as organizations increasingly shift to value-based care. And there’s a reason: in payment structures that prioritize value, neglecting HCCs can yield substantial consequences.
An inadequate understanding of HCCs may hinder healthcare providers in their efforts to maximize reimbursements and succeed in value-based care models. By potentially causing errors in patient classification, incomplete reporting of chronic ailments, and overlooking chances for effective risk adjustment, inaccurate HCC coding can lead to reimbursement failures. When healthcare providers can not accurately depict the seriousness of their patients’ health conditions, it can ultimately result in diminished financial support for them.
So, how should healthcare organizations go about improving their understanding of HCC coding and optimizing their success within value-based care models? In this blog, we will delve deeper into the world of HCC coding and its pivotal role in achieving success within the domain of value-based care.
Hierarchical Condition Category (HCC): Understanding the Basics
Hierarchical Condition Category (HCC) coding is a system used in healthcare to classify and document the severity of a patient’s medical conditions for billing and reimbursement purposes. It assigns risk scores using ICD-10-CM codes and demographic data to calculate a risk adjustment factor (RAF) score for each patient. The higher the risk score, the more resources and care a patient is likely to require.
In the context of Medicare Shared Savings Programs (MSSP), this algorithm influences the reimbursement that healthcare providers receive to efficiently manage their patients’ health. Accurate HCC coding aids in risk adjustment, ensuring that fair compensation is received for caring for sicker, more complex patients in MSSP. In other words, proper coding is indispensable for providers to receive the necessary resources and reimbursement in shared savings programs, ultimately leading to improved patient outcomes.
Risks of Inadequate HCC Coding
In value-based care arrangements, precise risk categorization plays a substantial role in determining your financial outcome, particularly when you’re taking on risk through value-based care agreements. Coding and documenting patients’ conditions accurately allows providers to demonstrate the severity of their patients’ illnesses and allocate resources effectively for care coordination, preventive services, and disease management.
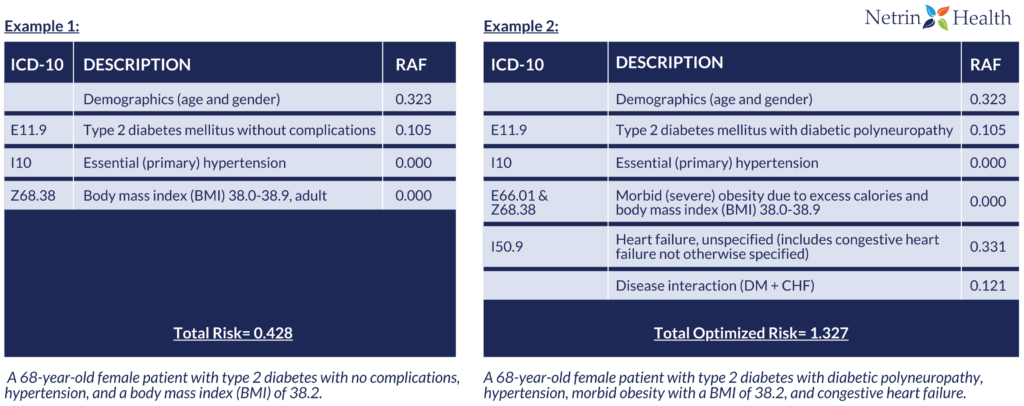
As illustrated in the tables above, the difference between coding a patient solely for type 2 diabetes and hypertension without complications and coding for additional conditions such as diabetic polyneuropathy, morbid obesity, and congestive heart failure can significantly impact the patient’s RAF score. A precise RAF score not only reflects the patient’s health status more comprehensively but also ensures that healthcare providers receive adequate reimbursement for the complexity of care required, ultimately enhancing the quality of healthcare delivery.
HCC Coding Reminders
- Risk adjustment scores reset annually, necessitating the reporting of active diagnoses, including chronic conditions, each year, often accomplished during the annual wellness visit. Preventive screenings, like assessing depression risk factors, help identify additional diagnoses influencing a patient’s risk.
- HCCs are cumulative, stressing the importance of coding all concurrent conditions during the encounter that impact patient care and treatment.
- Avoid coding past treated conditions that have resolved, using history codes as secondary codes only when they affect current care or treatment.
- Documentation must substantiate reported diagnoses, adhering to the MEAT Principle: diagnoses should be monitored, evaluated, assessed, or treated. Unsupported diagnoses won’t withstand audits, so ensure coding aligns with ICD-10-CM guidelines.
- Code with utmost specificity, correctly sequencing diagnoses on the claim. Consider factors such as type, underlying cause, control status, severity, site, associated comorbid conditions, and substance use/exposure when selecting the appropriate diagnosis code.
Using the MEAT Principle
The “MEAT” principle in HCC coding stands for “Monitor,” “Evaluate,” “Assess,” and “Treat“.
The MEAT principle serves as a fundamental guideline for accurately capturing the severity of a patient’s medical conditions. It emphasizes that for a diagnosis to be valid and count towards the patient’s Risk Adjustment Factor (RAF) score, it must be actively monitored, evaluated, assessed, and treated over a specific time frame. This principle ensures that HCC codes reflect ongoing medical management and are not based on historical or trivial diagnoses, contributing to a more accurate and comprehensive representation of a patient’s health status for proper risk adjustment and healthcare reimbursement.

In the evolving landscape of healthcare, accurate HCC coding is the linchpin for success in MSSP programs and value-based care initiatives. It’s the key to a fair and equitable compensation model that aligns with the complexity of patients’ health conditions. More importantly, precise HCC coding empowers healthcare providers to deliver tailored, high-quality care, ensuring that patients receive the right interventions, while also enhancing the overall effectiveness and sustainability of value-based care approaches. It’s a cornerstone that cannot be overlooked in the pursuit of a healthier, more patient-centric future.
For more information on optimizing HCC coding for value-based care, please don’t hesitate to contact us at info@netrinhealth.com or call us at 571-489-7777. We’re here to help you navigate the path to better healthcare outcomes.
