Share Article
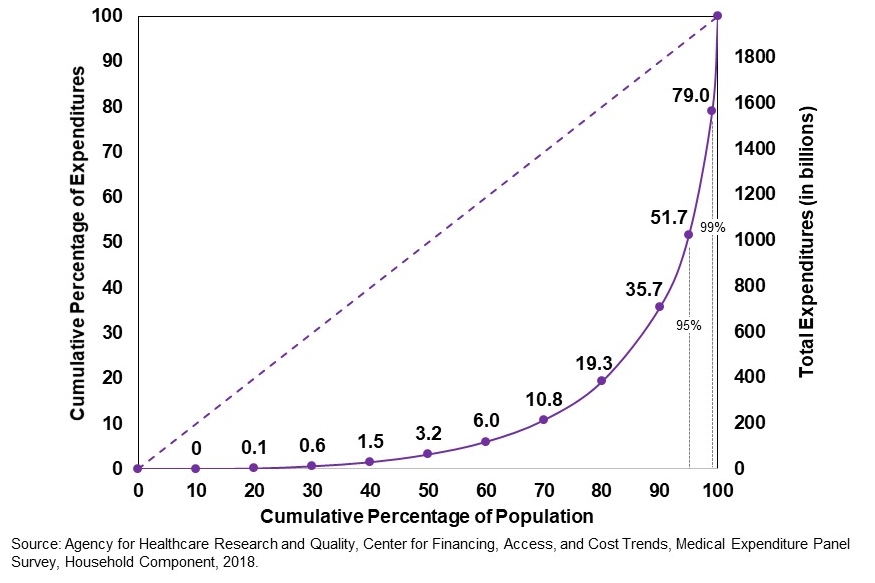
Today, 1% of patients account for more than 20% of health care expenditures, and 5% account for nearly half of the nation’s spending on health care (Figure 1). High-need high-cost (HNHC) patients are defined in the literature as the small subgroup of the population that accounts for the majority of US health care costs. In accountable care organizations, the main focus is developing care management programs to improve care and thereby control costs for those patients. Many programs target “high-need, high-cost” patients who have multiple chronic conditions and comorbidities. The care management team targets an acute episodic event, an ongoing unstabilized chronic condition and behavioral health management to prevent ER or IP utilization. There is a challenge to address socioeconomic need, social support, and social isolation.
Complex care management (CCM) programs have emerged as a favorable model to better care for high-need, high-cost patients. It includes a set of activities designed to more effectively help patients and their caregivers in managing medical conditions and psychosocial factors. CCM is usually provided to patients who have significant medical needs and often experience a high number of emergency room visits or hospitalizations. The goal is to improve the patient’s overall health status, stabilize an ongoing chronic condition and reduce the need for emergency room utilization and hospital admissions.
In recent years, complex care management programs have been extensively adopted by health systems and delivery organizations entering value-based payment setting. In fact, a 2018 survey found that 96% of accountable care organizations had implemented complex care management programs for high-need, high-cost patients.
Complex care management has resulted a 22% reduction in costs and a 21% reduction in hospitalizations.
– The American Journal of Managed Care –
A complex care management program reduced spending and inpatient utilization among high-need, high-cost Medicaid patients, as the result of a study published in American Journal of Managed Care study has shown. Another study that has been published in the July issue of the American Journal of Managed Care verified that complex care management is having a significant positive impact on both clinical and financial outcomes in accountable care organizations participating in the Next Generation (Next Gen) ACO program. In fact, the study demonstrated that complex care management has led to 22% reduction in healthcare costs and a 21% reduction in hospitalizations.
Multiple potential mechanisms could explain the remarked decreases in utilization and spending. Improved management of medical, social, and behavioral risk factors prevent acute increasing of chronic disease. Patient activation and engagement leads to improved self-management and adherence. Eventually, social and behavioral balance promotes safe discharge planning, reducing the need or duration of hospital admissions.

Netrin Health, as part of the Medicare Shared Savings Program, has 36000 lives engaged and saved more than $14 million for the Centers for Medicare & Medicaid Services under various value-based care programs. Netrin Health is not only an MSSP program, but also a care transformation organization with advance innovative MDPCP program.
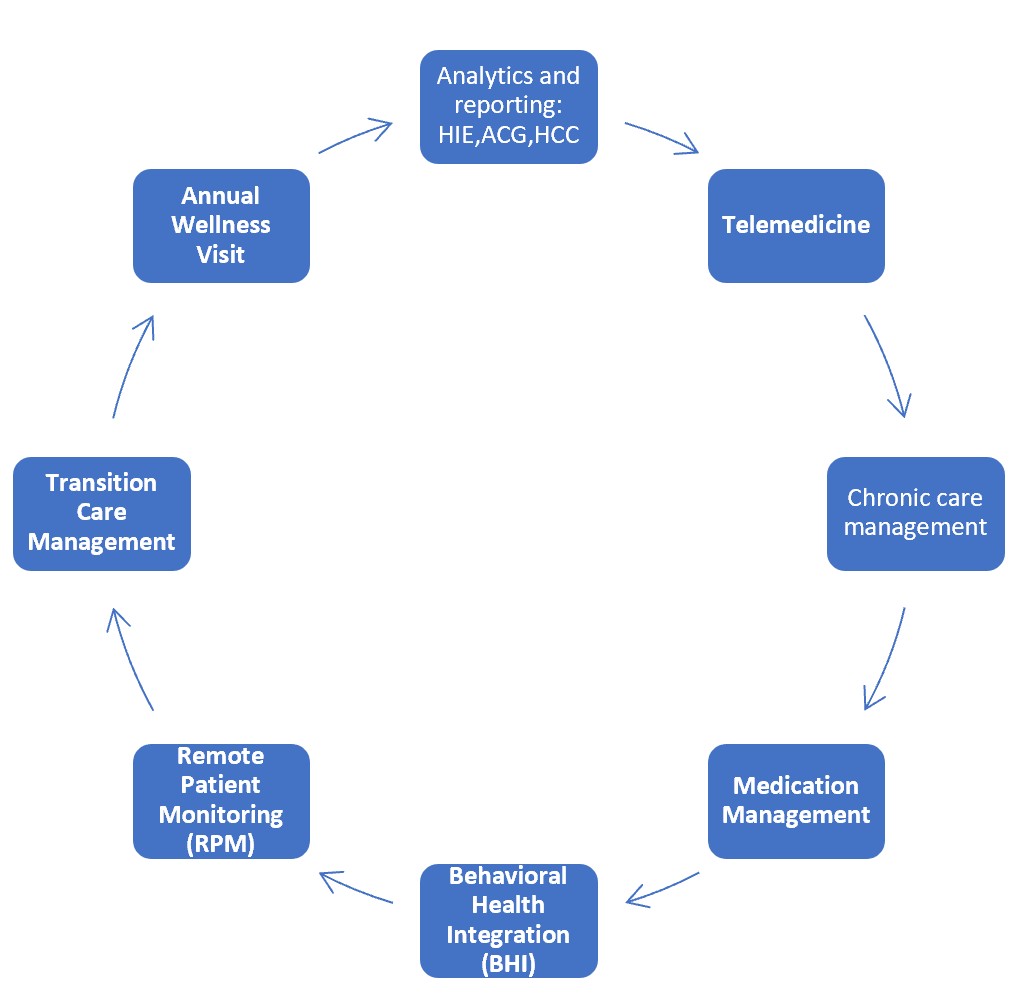
We deploy different mechanisms to find and predict which patients might need to be selected and screened for complex care management. These strategies include advance predictive analytics, HCC risk scores, and adult risk stratification tool based on best evidence practice. Chronic Care Management uses all the advance tools like text messaging, Person APP and Remote Patient Monitoring to engage patients and maintain 95-98% compliance in the Netrin Chronic Care Management Program.
Conclusion
Improving care quality and lowering expenditures for the population have become a focus for policy makers, clinicians, payers, and health systems. One of the important areas to focus is to reach out these goals is complex care management. At Netrin Health, we focus on health equity related Chronic Care Management programs in which specially trained, multidisciplinary teams coordinate closely with primary care teams to meet the needs of patients with multiple chronic conditions or advanced illness, many of whom face barriers in accessing health services. We use different types of care management interventions well integrated with SDOH screening, which perform comprehensive health assessment to identify and engage patients who are at high risk for unnecessary utilization and poor outcomes. We have worked with our primary care practices to not only reduce hospitalizations and readmissions but also address social needs for high acuity patients for our CPC + models, PMO models, MCO models and FQHC’s.
Contact us today to learn more about our Chronic Care Management and other value-based care programs.
Bilazarian, A. (2021, January). High‐need high‐cost patients: A Concept Analysis. In Nursing Forum (Vol. 56, No. 1, pp. 127-133).
Hong, C. S., Siegel, A. L., & Ferris, T. G. (2014). Caring for high-need, high-cost patients: what makes for a successful care management program?
Powers, B. W., Modarai, F., Palakodeti, S., Sharma, M., Mehta, N., Jain, S. H., & Garg, V. (2020). Impact of complex care management on spending and utilization for high-need, high-cost Medicaid patients. Am J Manag Care, 26(2), E57-E63.
Long, P., Abrams, M., Milstein, A., Anderson, G., Apton, K. L., Dahlberg, M., & Whicher, D. (2017). Effective care for high-need patients. Washington, DC: National Academy of Medicine.
Peck KA, Usadi B, Mainor A, Newton H, Meara E (2018). How ACOs are caring for people with complex needs. The Commonwealth Fund website. commonwealthfund.org/publications/fund-reports/2018/dec/how-acos-arecaring-people-complex-needs. Accessed Feb 1, 2022.
O’Hara, N., Tran, O. C., Phatakwala, S., Cattrell, A., & Ajami, Y. (2020). Effective Care Management by Next Generation Accountable Care Organizations. The American Journal of Managed Care, 26(7), 296-302.
