Share Article
The World Health Organization defines health as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity”. Because mental health is vital to overall health and well-being, it must be recognized and treated in all Americans, including senior adults, with the same urgency as physical health. For this reason, mental health is becoming a more important part of the public health journey.
Mental Health Problems in Older Adults
It is estimated that 20% of people aged 55 years or older experience some type of mental health concern. The most common conditions include anxiety, severe cognitive impairment, and mood disorders (such as depression or bipolar disorder). Mental health issues are also often connected as a factor in cases of suicide. Older men have the highest suicide rate of any age group. The significance of depression, a type of mood disorder, is the most widespread mental health problem among senior adults. It is associated with grief and suffering. It also can lead to defacement in physical, mental, and social functioning. Older adults with depression visit the doctor and emergency room more often, use more medication, induce higher outpatient charges, and length of stay in the hospital.
Importance of Screening – PHQ-9 within Primary Care
A mental health screening is an exam of your emotional health and helps you identify a mental health disorder. Screening evaluates risk factors, which can be genetic, behavioral, or environmental. Screenings are valuable, because they grant early identification and intervention, leading to better outcomes. Screenings may also reduce long-term disability, preventing years of suffering. In addition, benefits include distinguishing between those who could benefit from slight intervention and others who may need further diagnostic assessment or possible treatment, especially for common mental disorders like depression.
Efforts to improve depression identification and treatment in primary include increased use of screening tools. The Patient Health Questionnaire (PHQ)–2 and PHQ-9 are the most commonly used adult depression screening tools and display clinical advantage with diagnostic accuracy. The PHQ-2 was designed to be used as the first step in the screening process and if positive, to be followed with the more comprehensive PHQ-9. The PHQ-9 consists of 9-items based on the 9 DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, fifth edition) criteria for major depressive disorder. Meta-analysis of pooled data from 14 760 primary care adults with depressive disorder found both PHQ-2 and PHQ-9 to be effective, valid, and reliable for identifying depression in primary care.
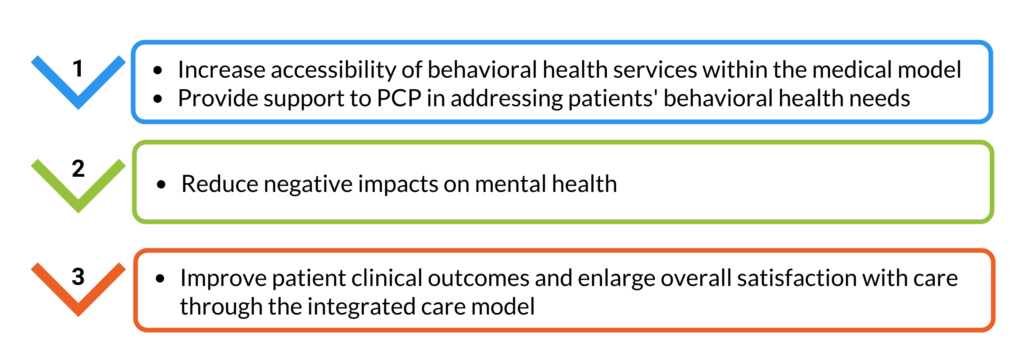
Integrated Behavioral Health in Primary Care
Providers practicing integrated behavioral health care acknowledge that both medical and behavioral health factors are important parts of a person’s general health. Medical and behavioral health clinicians work together as a team to address a patient’s distress. Care is delivered by these integrated teams in the primary care setting unless patients request specialty services. The benefit is better communication and adjustment, while working toward one set of overall health goals. To address overall health concerns, integration of behavioral health services into the clinical primary care setting is suggested to:
Reducing behavioral health related ER visits
A new analysis from the Colorado All Payer Claims Database (CO APCD) shows that over 17,000 Coloradans visiting an Emergency Department (ED) from 2016-2018 had a primary diagnosis related to mental health.
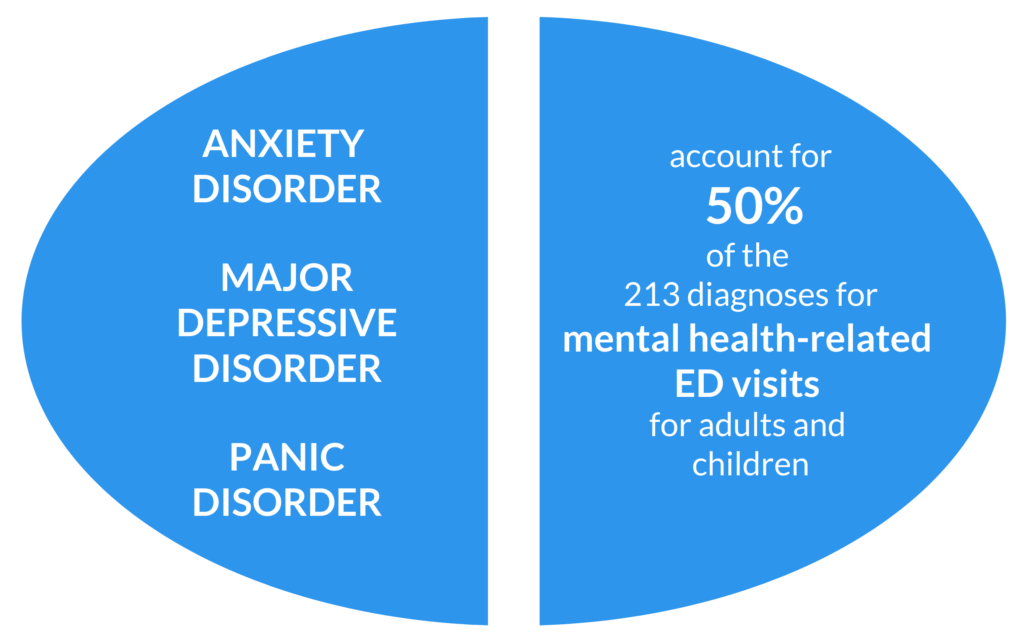
Research shows that receiving integrated behavioral health can reduce hospitalization and ED utilization. A study compared patients in a safety net primary care clinic who received integrated behavioral health services to those who did not receive such services. It found a significant decrease in preventable hospitalizations in the year after behavioral health intervention. Another study has also found that using collaborative care among patients with acute cardiac illness and depression/anxiety was associated with reduced ED utilization.
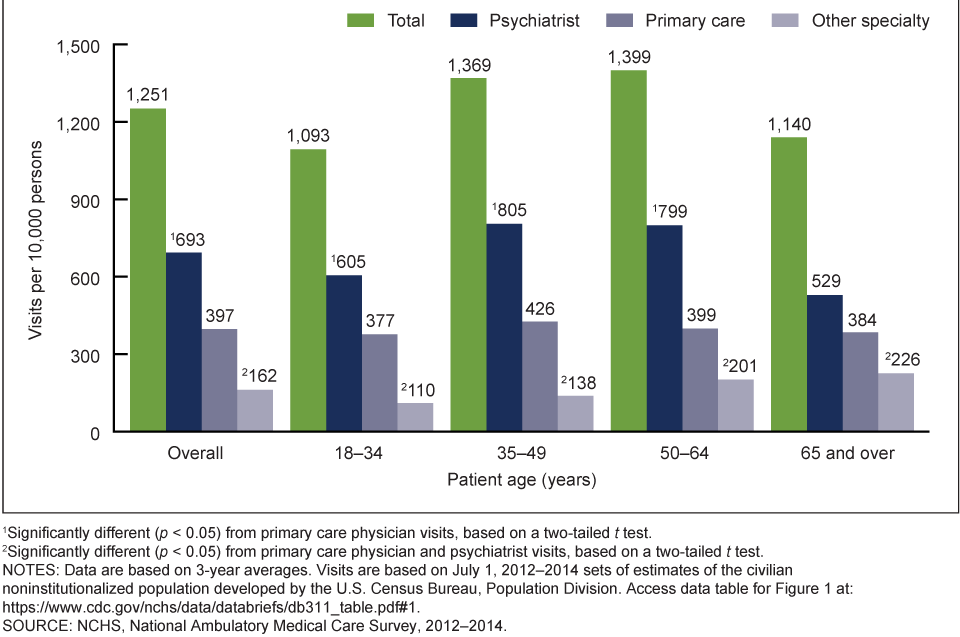
Access to Mental Health Care
The demand for mental health services is stronger than ever, with nearly six in 10 (56%) Americans search or want to seek mental health services. The large majority of Americans (76%) also believe mental health is just as important as physical health. These beliefs are driven by various perceived barriers in Americans’ ability to quest mental health treatment, as shown below.

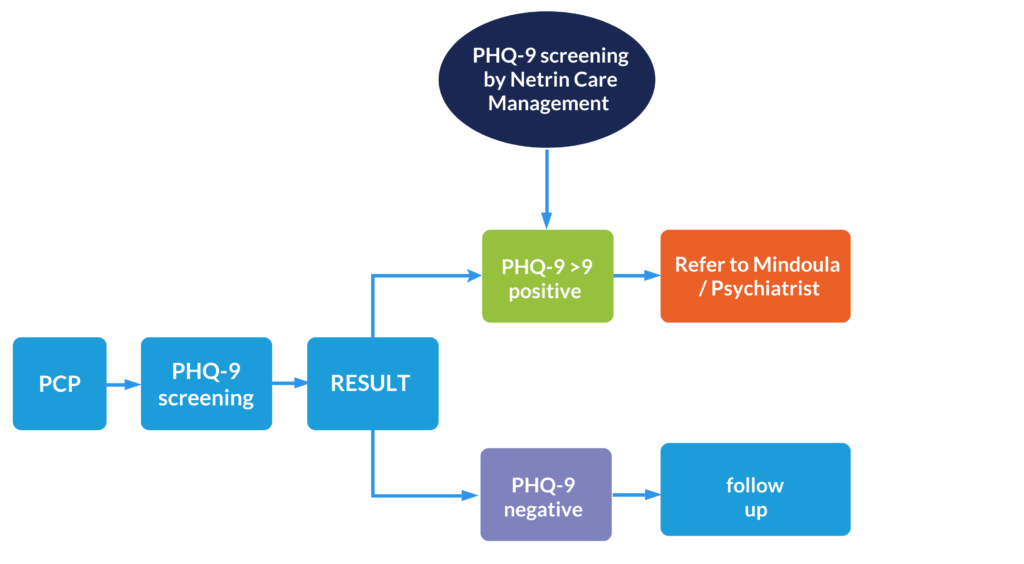
Netrin Health’s Integrated Behavioral Health Model
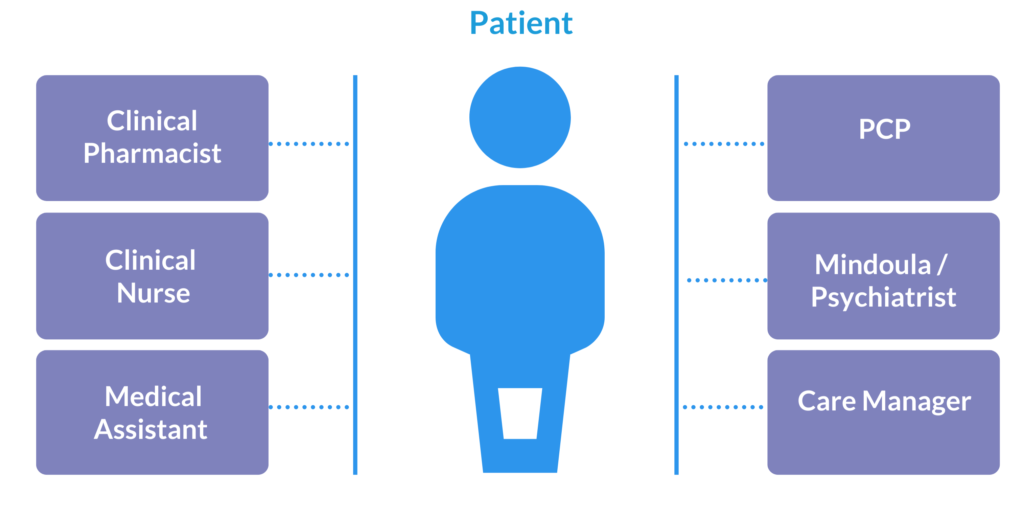
Netrin Health has the expertise and connections to guide primary care practices to integrate the behavioral health model that best fits their patients’ needs. Whether patients want to add a therapist in office or build a collaborative relationship with a psychiatrist off-site as shown in the flow chart, Netrin Health will help meet the needs of them. Netrin is also collaborating with Mindoula (a next generation population health management company that identifies, engages, and serves populations with complex behavioral health, medical, and social challenges across the continuum of care) which allows treating mild-to-moderate mental health and substance use disorders, identifying undiagnosed high-risk patients before they become high-cost patients, and improving HCC coding.
Netrin’s Depression Screening and Referral Flow Chart
Netrin Health Behavioral Health Model
Conclusion
Nearly 1 in 5 Americans has some type of mental health condition. Spending on mental health treatment has risen in recent years includes therapy and prescription medications as well as stays in psychiatric or substance abuse rehabilitation centers. Mental health screenings grant early detection and intervention and help out the gap. Screening for early identification and treatment of mental health disorders in primary care settings can improve quality of life, reduce health care spending and also complications from untreated mental health disorders.
For further details about our value-based care programs, contact us today.
World Health Organization (WHO), Accessed Feb 23,2022.
Centers for Disease Control and Prevention. (2008). The state of mental health and aging in America. URL: https://www. CDC. gov/aging/pdf/mental health. pdf [accessed 2020-06-09]. Accessed Feb 23,2022.
Siniscalchi, K. A., Broome, M. E., Fish, J., Ventimiglia, J., Thompson, J., Roy, P., … & Trivedi, M. (2020). Depression screening and measurement-based care in primary care. Journal of primary care & community health, 11, 2150132720931261.
Agency for Healthcare Research and Quality. What is Integrated Behavioral Health? URL: https://integrationacademy.ahrq.gov/about/integrated-behavioral-health. Accessed Feb 23,2022.
Center for Improving Value in Health Care. New Analysis Shows Frequency of Mental Health-Related ED Visits. Accessed Feb 23,2022.
Serrano, N., Prince, R., Fondow, M., & Kushner, K. (2018). Does the primary care behavioral health model reduce emergency department visits? Health services research, 53(6), 4529-4542
National Council for Mental wellbeing. New Study Reveals Lack of Access as Root Cause for Mental Health Crisis in America. Accessed Feb 23,2022.
